FOR IMMEDIATE RELEASE
What They’re Saying: Rep. Green Seeks to Reform Prior Authorization
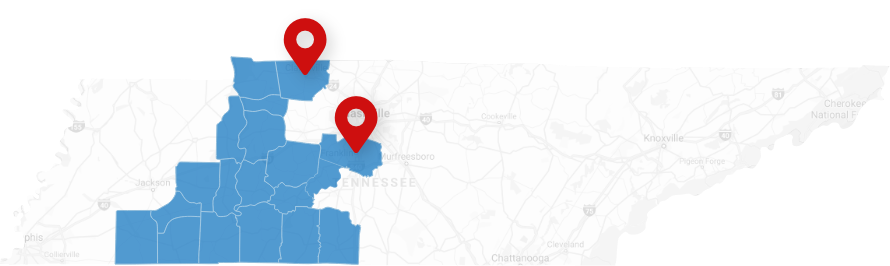
WASHINGTON—This week, Rep. Mark Green, M.D. re-introduced his Reducing Medically Unnecessary Delays in Care Act of 2025, alongside Rep. Greg Murphy (R-NC) and Congressional Democratic Doctors Caucus Co-chair Kim Schrier, M.D. (D-WA) to address the use of prior authorization requirements in Medicare, Medicare Advantage, and Part D prescription drug plans.
The Reducing Medically Unnecessary Delays in Care Act would reform the practice of prior authorization in Medicare and Medicare Advantage by requiring that board-certified physicians in the same specialty are the ones making these important decisions. It would also direct Medicare, Medicare Advantage, and Medicare Part D plans to comply with requirements that restrictions must be based on medical necessity and written clinical criteria, as well as additional transparency obligations.
What They’re Saying…
“On behalf of the physician and medical student members of the American Medical Association (AMA), I am pleased to express our support for H.R. 2433, the ‘Reducing Medically Unnecessary Delays in Care Act of 2025.’ [...] PA determinations made by individuals lacking appropriate clinical expertise not only undermine the treating physician’s clinical judgment but also introduce inefficiencies that fall disproportionately on private medical practices, especially smaller or independent ones that lack the administrative infrastructure to absorb the high costs of compliance and fighting inappropriate denials. These burdens translate into real-world harm including delayed diagnoses, treatment interruptions, worsening conditions, and declining patient trust.”
-American Medical Association CEO and Executive Vice President James L. Madara, MD
Read the full letter here.
“The overuse of prior authorization is a persistent obstacle that prevents patients from receiving quality care from their physicians. Often, prior authorization requests are reviewed—and denied—by insurance company representatives who lack the medical expertise to appropriately judge what level of care is necessary for a patient. This welcome legislation would require the reviewers to be physicians with actual experience in the field of medicine they are passing judgment over. Our patients deserve no less.”
-American Medical Association President Bruce A. Scott, M.D.
"This bill takes an important step toward reforming prior authorization processes that continue to impose unnecessary delays and administrative burdens on physicians and patients by requiring that determinations about medical necessity are made by board-certified physicians with clinical experience in the same specialty as the ordering physician."
-American Medical Association CEO and Executive Vice President James L. Madara, MD
Read the full letter here.
“The American College of Physicians strongly opposes prior authorization requirements that are overly burdensome and pull physician time away from where it should be, on caring for our patients. These bureaucratic delays in care are especially galling when decisions about needed care are not being reviewed by physicians who are trained and knowledgeable in that care. Reforms that seek to make the prior authorization process more transparent, like those proposed in the Reducing Medically Unnecessary Delays in Care Act of 2025, are critical to ensuring that our nation’s seniors are able to access the care that they need when they need it most.”
-American College of Physicians President Isaac O. Opole, MBChB, PHD, MACP
"The AOA appreciates Congressman Green’s effort to reintroduce the Reducing Medically Unnecessary Delays in Care Act, which will help ensure patients can access the care their physician deems necessary. Osteopathic physicians take a patient-centered, whole-person approach to health care, yet overly burdensome prior authorization processes often create significant barriers to effective care delivery. To ensure a true peer-to-peer review, prior authorization reviews must be conducted accurately and exclusively by physicians within the same specialty, preventing unnecessary delays and ensuring patients receive the most appropriate care."
-American Osteopathic Association President Teresa A. Hubka, DO, FACOOG (Dist.)
"The AOA applauds Rep. Green's leadership in ensuring that harmful PA practices do not delay access to care. Reforming PA in traditional Medicare, Medicare Advantage, and Part D by requiring prior authorizations and adverse determinations to be made by a licensed physician who is board certified in a relevant specialty is an essential step toward re-empowering the physician-patient relationship."
-American Osteopathic Association President Teresa A. Hubka, DO, FACOOG (Dist.) and American Osteopathic Association Interim Chief Executive Officer Kathleen S. Creason, MBA
Read the rest of the letter here.
“The American College of Osteopathic Family Physicians (ACOFP) applauds Representative Green for re-introducing the Reducing Medically Unnecessary Delays in Care Act. This critical legislation will put patients first and ensure that the doctor-patient relationship is preserved by addressing an insurer’s use of prior authorization requirements. This will ensure that physicians, including osteopathic family physicians, are the ultimate decision makers concerning their patient’s course of treatment, rather than insurers. The Reducing Medically Unnecessary Delays in Care Act will reduce delays in care and increase patient access to health care items and services, therefore improving health outcomes.”
-American College of Osteopathic Family Physicians President Brian A. Kessler, DO, FACOFP (Dist.)
“The National Infusion Center Association (NICA) applauds Representative Mark Green's reintroduction of the Reducing Medically Unnecessary Delays in Care Act of 2025. This critical legislation addresses the urgent need to reform prior authorization processes within Medicare and Medicare Advantage, ensuring that these vital decisions are made by qualified medical professionals with the necessary expertise. NICA firmly believes that patients deserve timely access to the treatments prescribed by their physicians, and this bill represents a significant step towards eliminating unnecessary barriers to care.”
-The National Infusion Center Association (NICA)
"Rural Health Clinics across the country rank the administrative burdens associated with prior authorizations as the #2 most concerning issue for their facilities. We thank Dr. Green, Dr. Schrier, and Dr. Murphy for their leadership on H.R.2433 to help ensure that patients, like those served by RHCs, have access to timely services.”
-National Association of Rural Health Clinics Director of Government Affairs Sarah Hohman, MPH, CRHCP
“As patient and physician advocates, the Alliance of Specialty Medicine (the “Alliance”) writes in support of your legislation, H.R. 2433, the Reducing Medically Unnecessary Delays in Care Act, which would ensure that prior authorization decisions in Medicare and Medicare Advantage are made by board-certified physicians in the same specialty as the physician of the treatment or disease in question, and direct plans to comply with requirements around medical necessity and written clinical criteria.The Alliance represents more than 100,000 specialty physicians and surgeons across 16 specialty and subspecialty societies and is deeply committed to improving access to specialty medical care through the advancement of sound health care policy. The Alliance urges Congress to meaningfully improve the prior authorization process, to reduce administrative burdens, and ensure safe, timely, and affordable access to care for patients, as proposed in the Reducing Medically Unnecessary Delays in Care Act.”
-The Alliance of Specialty Medicine
Read the rest of the letter here.
“On behalf of the undersigned members of the Regulatory Relief Coalition (RRC), a coalition of national physician organizations seeking to reduce regulatory burdens that interfere with patient care, we are pleased to support the Reducing Medically Unnecessary Delays in Care Act of 2025 (H.R. 2433). As a leading advocate for reforming prior authorization in the Medicare Advantage (MA) program on behalf of seniors and the physicians who care for them, the RRC applauds your leadership on this legislation to improve the prior authorization process in Medicare, MA, and Medicare Part D plans. [...] RRC members agree that only qualified medical personnel—ideally providers of the same medical specialty or subspecialty as the prescribing/ordering physicians—should make these decisions. Furthermore, we agree that prior authorization decisions should reflect evidence-based guidelines consistent with national medical specialty society guidelines where available and applicable.”
-Regulatory Relief Coalition
“A bill to reform prior authorization requirements for Medicare Advantage (MA)—a massive burden that nursing home operators have been trying to change for some time—was reintroduced on Capitol Hill… Nursing homes have long argued that this aspect of MA needs to be right-sized through legislation. [...] The Reducing Medically Unnecessary Delays in Care Act of 2025 seeks to reform prior authorization for Medicare and Part D prescription drug plans in addition to MA…”
-Amy Stulick, Skilled Nursing News
Read more here.
“The American College of Allergy, Asthma and Immunology’s (ACAAI’s) Advocacy Council is pleased to share this letter [...] expressing our support for the Reducing Medically Unnecessary Delays in Care Act of 2025. Administrative burdens like prior authorizations take valuable time away from patient care and contribute to physician burnout. This bill is an important step in reducing these burdens and will enable allergists to focus on providing timely, high-quality care. [...] Allergy patients face daily care disruptions and denials due to overburdening and excessive prior authorization requirements. Allergy practices must dedicate a large portion of staff and financial resources to comply with these requirements. ACAAI’s Advocacy Council appreciates that this bill ensures that board-certified allergists/immunologists will be tasked with evaluating prior authorization requests from allergists/immunologists. This approach helps balance the use of prior authorizations in limited cases while ensuring that the most qualified experts assess these requests. ACAAI’s Advocacy Council supports this bill’s approach to standardizing prior authorization processes and criteria across Medicare plans. […] This approach will help streamline the prior authorization process so doctors can instead direct their attention to where it belongs: caring for patients.”
-American College of Allergy Asthma and Immunology President James M. Tracy, DO, FACAAI & American College of Allergy Asthma and Immunology Advocacy Council Chair Travis A. Miller, MD, FACAAI
Read the letter here.
“The Healthcare Business Management Association (HBMA) is pleased to share this letter [...] expressing our support for the Reducing Medically Unnecessary Delays in Care Act of 2025. Administrative burdens like prior authorizations take valuable time away from patient care and contribute to physician burnout. This bill is an important step in reducing these burdens and will enable medical practices to focus on providing timely, high-quality care. [...] Medical practices face daily care disruptions and denials due to overburdening and excessive prior authorization requirements. Medical practices must dedicate a large portion of staff and financial resources to complying with these requirements. If passed, this bill would require board-certified clinicians with relevant medical backgrounds adjudicate prior authorization requests. This approach ensures qualified medical experts assess these requests, not algorithms.”
-Healthcare Business Management Association President Kirk Reinitz
Read the letter here.
“On behalf of The Society of Thoracic Surgeons (STS), I would like to thank you for introducing H.R. 2433, the Reducing Medically Unnecessary Delays in Care Act. Founded in 1964, STS is a not-for-profit organization representing more than 7,800 surgeons, researchers, and allied healthcare professionals worldwide who are dedicated to ensuring the best possible outcomes for surgeries of the heart, lungs, and esophagus, as well as other surgical procedures within the chest. We deeply appreciate your leadership on this legislation that aims to reform prior authorization requirements in Medicare, Medicare Advantage, and Part D prescription drug plans. As you know, the overuse of prior authorization is often a roadblock that prevents physicians from treating patients in a timely manner, if at all. Prior authorization can delay care and increase costs without improving patient outcomes.”
-Society of Thoracic Surgeons (STS) President Joseph F. Sabik III, MD
Read the letter here.
"Rep. Green's legislation is a positive step towards eliminating these burdens and restoring clinical decisionmaking to where it belongs – between doctor and patient. The requirement that MA plans use licensed specialists to make clinical preauthorization and coverage determinations is a commonsense reform that will reduce unwarranted denials and save providers time. Furthermore, the provision of the bill requiring MA plans to issue written, online criteria for preauthorization that are in line with clinical standards will increase transparency and ensure that patients are getting care without unnecessary delay."
-Ascension Senior Vice President of Public Affairs Amy Efantis
Read the letter here.
Read more from Dave Muoio in Fierce Healthcare, Ashleigh Fields in The Hill, Kaitlin Housler in the Tennessee Star, in ClarksvilleNow, or in Becker’s Hospital Review.
This bill was co-sponsored by Reps Greg Murphy (R-NC), John Joyce (R-PA), Rich McCormick (R-GA), Andy Harris (R-MD), Kim Schrier (D-WA), Tim Burchett (R-TN), Brian Babin (R-TX), Mariannette Miller-Meeks (R-IA), Mike Kennedy (R-UT), Pat Harrigan (R-NC), Beth Van Duyne (R-TX), Ronny Jackson (R-TX), Brad Finstad (R-MN), and Neal Dunn (R-FL)
This bill was endorsed by: American Medical Association, American Osteopathic Association, American College of Emergency Physicians, American College of Physicians, American Academy of Family Physicians, American College of Gastroenterology, American Academy of Otolaryngology, American Association of Orthopedic Surgeons, American College of Osteopathic Family Physicians, Oncology Nursing Society, Medical Group Management Association, National Infusion Center Association, Infusion Access Foundation, Alliance of Specialty Medicine, American Academy of Facial Plastic and Reconstructive Surgery, American Academy of Otolaryngology—Head and Neck Surgery, American Association of Neurological Surgeons, American College of Mohs Surgery, American Gastroenterological Association, American Society of Cataract and Refractive Surgery, American Society of Dermatologic Surgery Association, American Society of Echocardiography, American Society of Plastic Surgeons, American Society of Retina Specialists, American Urological Association, Coalition of State Rheumatology Organizations, Congress of Neurological Surgeons, National Association of Spine Specialists, Society of Interventional Radiology, Society for Cardiovascular Angiography and Interventions, and National Association of Rural Health, American College of Asthma, Allergy, and Immunology, and Healthcare Business Management Association.
Read the bill here.
Read more about the Reducing Medically Unnecessary Delays in Care Act here.
###